When patients hear the phrase dental bone graft, the initial thought is often of a highly technical, complex surgical procedure. Yet at its core, a dental bone graft is a restorative treatment designed to replace or regenerate lost bone in the jaw, often in preparation for dental implants or to preserve facial structure. To answer directly: yes, a dental bone graft is a treatment that provides patients with stronger bone support, most commonly when tooth loss, periodontal disease, or trauma has caused significant bone deterioration. Within the first hundred words, the essence is clear—dental bone grafting is not cosmetic alone; it is a foundation-building step for oral health and long-term stability. Patients are increasingly asking about how it works, its recovery process, types, risks, and success rates. This article aims to provide readers with a deep and updated understanding, helping them navigate a procedure that is growing in popularity due to its reliable outcomes and its role in modern restorative dentistry.
Bone grafting has advanced considerably in the last two decades. Where once it was seen as a daunting surgery reserved for severe cases, new biomaterials, minimally invasive techniques, and faster healing protocols have made it far more accessible. Dentists and oral surgeons now use grafting not only to prepare jaws for implants but also to stabilize dentures, repair trauma injuries, and address congenital defects. By the end of this article, readers will understand what a dental bone graft is, why it is done, what to expect, and how innovation is shaping its future.
What is a Dental Bone Graft?
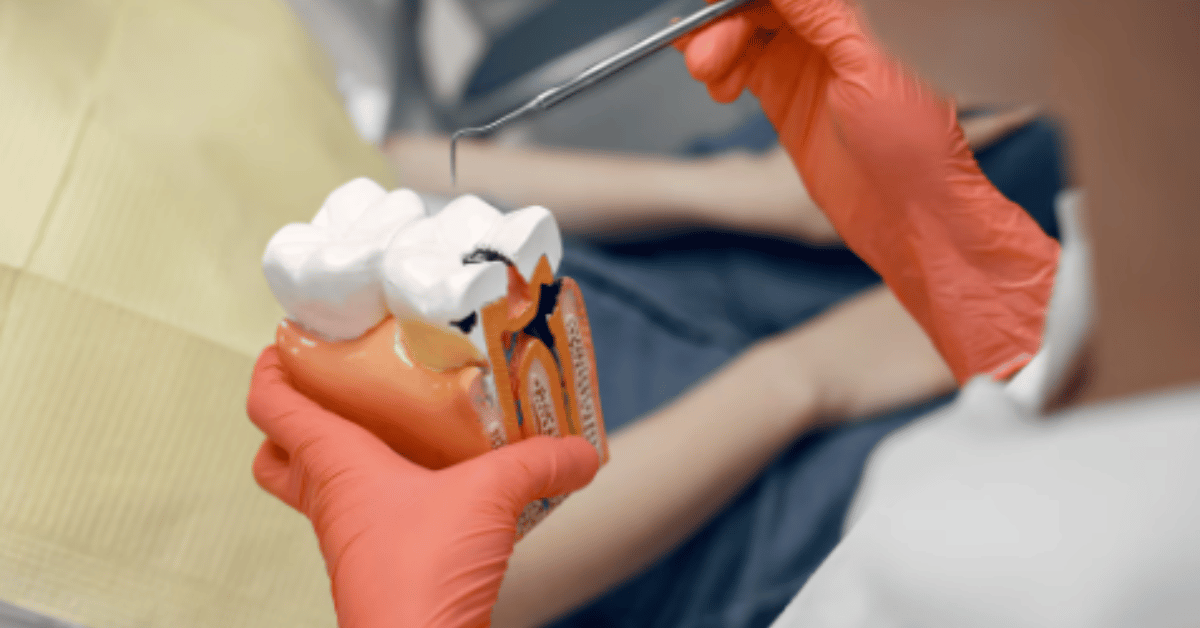
A dental bone graft is a surgical technique that replaces missing bone in the jaw with either natural bone tissue from the patient or artificial substitutes. The goal is to allow new bone growth, ultimately strengthening the jaw’s structure and creating a stable base for dental implants or prosthetics. Without adequate bone density, implants cannot be anchored, and even natural teeth may loosen over time.
There are several types of grafts. Autografts use the patient’s own bone, typically harvested from areas like the hip or chin. Allografts use donor bone from human tissue banks. Xenografts rely on animal sources, usually bovine bone that has been processed and sterilized. Synthetic options, known as alloplasts, use materials such as calcium phosphates. Each option has unique benefits, costs, and healing times. The procedure can vary depending on whether the graft is small, performed immediately after tooth extraction, or larger, requiring staged surgeries.
Why Do Patients Need a Dental Bone Graft?
The most common reason for a dental bone graft is preparation for dental implants. Tooth loss, especially over long periods, leads to bone resorption—where the jawbone naturally shrinks due to lack of stimulation from chewing. Studies suggest that within one year of tooth loss, up to 25% of bone width can be lost. A graft helps restore lost volume, allowing implants to integrate successfully.
Other reasons include periodontal disease, which erodes supporting bone, leaving teeth unstable. Trauma from accidents, cyst removal, or congenital deformities can also result in bone deficits requiring grafts. In addition, some patients undergo grafting to improve the aesthetics of their smile by restoring the natural contour of the jawline. “A strong foundation is not just about implants,” one oral surgeon explained, “it is about preserving the integrity of the entire oral system.”
Types of Dental Bone Grafts
Dentists choose the type of graft depending on patient needs, health conditions, and budget. Below is a table outlining common categories:
Table 1: Types of Dental Bone Grafts
| Type of Graft | Source | Advantages | Limitations | Typical Use Case |
|---|---|---|---|---|
| Autograft | Patient’s own bone | High compatibility, no rejection | Requires second surgery, more recovery time | Major bone loss cases |
| Allograft | Human donor | Abundant supply, avoids second surgery | Slight risk of rejection, slower integration | Periodontal repair, ridge preservation |
| Xenograft | Animal bone (bovine) | Long-term volume stability | Integrates slower | Implant preparation |
| Alloplast | Synthetic materials | No disease risk, customizable | May resorb quickly | Small defects, socket grafts |
This categorization demonstrates that there is no one-size-fits-all solution. Instead, graft choice depends on balancing biological compatibility, cost, healing time, and the ultimate goal of treatment.
The Procedure: Step by Step
Bone graft surgery begins with a thorough consultation, where imaging techniques like CT scans measure bone density. Once a treatment plan is developed, the patient undergoes anesthesia—local for minor grafts or sedation for more extensive ones. The dentist or surgeon then makes an incision in the gum, exposes the bone, and places the grafting material. In some cases, membranes or plates are used to stabilize the graft and guide regeneration. Sutures close the gum tissue, and healing begins. For small grafts, integration may take only a few months, but for larger reconstructions, full healing may extend to six to nine months. Patients usually return home the same day, but they must follow strict aftercare protocols, such as avoiding smoking, maintaining oral hygiene, and limiting pressure on the surgical site.
Recovery and Healing Expectations
Healing after a dental bone graft is gradual but highly predictable. Initial swelling and discomfort are normal for the first week, often managed with over-the-counter pain relievers and antibiotics. Soft diets are recommended to avoid disturbing the graft. By the second week, gum tissues typically heal well, though the bone underneath continues to regenerate for months.
The most critical phase is osseointegration, where the new graft material fuses with the natural bone. Success rates are remarkably high—studies show over 90% of grafts integrate successfully when patients follow proper post-surgical care. Smoking, uncontrolled diabetes, and poor oral hygiene are the most common risk factors for complications. “Patience is part of healing,” as one clinician often tells patients. “You may not see results immediately, but the foundation being built is for a lifetime.”
Risks and Complications
While safe, dental bone grafting does carry potential risks. Infection, graft rejection, nerve injury, and prolonged swelling are rare but possible complications. Pain beyond the normal recovery period may indicate graft failure, requiring revision surgery. Synthetic grafts sometimes resorb too quickly, failing to provide long-term stability. Patients can minimize these risks by choosing experienced providers, following strict aftercare guidelines, and disclosing complete medical histories. The overall consensus is that grafting is safer today than ever before, thanks to advanced sterilization, improved biomaterials, and minimally invasive techniques.
Costs and Insurance Coverage
The cost of dental bone grafting varies widely, influenced by graft type, complexity, and geographic region. Autografts are generally more expensive due to the need for two surgical sites, while synthetic grafts tend to be more affordable. Insurance often covers bone grafting if it is medically necessary, such as for trauma repair, but coverage for implant preparation is less consistent.
Table 2: Average Costs of Dental Bone Graft Procedures
| Graft Type | Average Cost (USD) | Insurance Coverage |
|---|---|---|
| Autograft | $2,500 – $3,500 | Often covered if medically necessary |
| Allograft | $1,200 – $2,500 | Sometimes covered |
| Xenograft | $1,000 – $2,000 | Rarely covered |
| Alloplast | $800 – $1,500 | Rarely covered |
For patients, understanding both the clinical and financial aspects of grafting is critical. A growing number of clinics offer financing plans, making these procedures more accessible.
Advances in Dental Bone Grafting
Modern dentistry is transforming how bone grafts are performed. Growth factors like platelet-rich plasma (PRP) and stem cell therapies accelerate healing and improve graft success rates. 3D-printed scaffolds, tailored to the patient’s anatomy, represent a cutting-edge development, enabling precision like never before. These technologies not only reduce healing time but also minimize complications. Furthermore, digital dentistry allows practitioners to simulate the procedure before surgery, giving patients a clear preview of outcomes. As one specialist put it, “The future of bone grafting lies not just in filling spaces but in regenerating living tissue.”
Patient Experience and Psychological Impact
Beyond the science, bone grafting has a profound psychological impact. Patients who once avoided smiling due to tooth loss or collapsed facial structures often regain confidence after successful grafting and implant placement. For many, the surgery is life-changing, restoring both function and identity. Patients describe the initial anxiety, but overwhelmingly note that the discomfort is temporary compared to the benefits. One patient explained, “I was nervous about surgery, but within months I could eat normally again and smile without hesitation. It gave me my life back.”
Conclusion
Dental bone grafting is no longer a procedure shrouded in medical jargon or fear. It is a routine, safe, and transformative option that allows patients to reclaim oral health, prepare for implants, and preserve natural structures. From types of grafts to recovery timelines, patients today have more options, higher success rates, and faster healing times than ever before. The key lies in informed decision-making. Patients should consult with qualified professionals, understand the graft materials available, and prepare for a healing process that demands patience but promises lasting results. As dental technology advances, grafting will only become more refined, offering not just restoration but true regeneration.
In the words of one oral surgeon: “When we rebuild bone, we rebuild lives.” Dental bone grafting exemplifies the convergence of science, artistry, and compassion in modern dentistry—ensuring that smiles remain strong, stable, and confident for decades to come.
FAQs
1. How long does it take for a dental bone graft to heal?
Healing typically takes 3 to 9 months, depending on the graft type and individual health factors.
2. Can dental bone grafts fail?
Yes, though rare. Failure can occur due to infection, smoking, or poor post-surgical care.
3. Is bone grafting painful?
Discomfort is common in the first week but is usually manageable with prescribed medications.
4. Do all implants require a bone graft?
Not always. Patients with sufficient bone density can receive implants without grafting.
5. Are synthetic bone grafts as effective as natural ones?
Synthetic grafts work well for small defects, but natural or donor bone often integrates more reliably in large cases.