Infiltration cortisone, often referred to simply as cortisone injection therapy, is one of the most widely used medical treatments for inflammatory conditions affecting joints, tendons, and soft tissues. It is designed to deliver targeted relief directly to the site of pain, inflammation, or swelling, providing patients with faster results compared to oral medication. Within the first 100 words, it is essential to clarify that infiltration cortisone is not a permanent cure but a therapeutic option that can significantly reduce symptoms of arthritis, tendonitis, bursitis, and even certain spinal problems. Patients often seek it when physical therapy, rest, or over-the-counter medications fail to provide adequate relief. What makes infiltration cortisone so important in modern medicine is its precision: instead of dispersing throughout the bloodstream like pills, it acts locally, addressing the root area of discomfort. For many individuals, this targeted approach restores mobility, reduces dependence on daily painkillers, and allows for a return to normal activities. Yet, while effective, the treatment comes with nuanced benefits, possible risks, and a need for proper medical evaluation, making it a subject worth exploring in depth.
What is Infiltration Cortisone?
Infiltration cortisone is a medical procedure where a corticosteroid solution is injected directly into an inflamed area of the body. These areas can include joints such as knees, hips, shoulders, or smaller regions like tendons and bursae. Corticosteroids are synthetic hormones that mimic cortisol, a natural hormone produced by the adrenal glands, known for its anti-inflammatory properties. By administering cortisone locally, physicians aim to reduce swelling, ease pain, and improve overall joint or tendon function. Unlike oral steroids that affect the entire body, infiltration targets a specific area, which minimizes systemic exposure while maximizing localized benefits. This method has been practiced for decades but has become more refined with advances in imaging techniques, such as ultrasound guidance, ensuring accuracy in needle placement. Importantly, while infiltration cortisone is often seen as a “quick fix,” it works best as part of a broader treatment plan, which may include physical therapy, lifestyle modifications, or surgery in severe cases.
Medical Conditions Treated with Infiltration Cortisone
The versatility of infiltration cortisone lies in its ability to address multiple inflammatory and painful conditions. The most common application is in osteoarthritis, particularly in large joints like the knee and hip, where degenerative changes often cause debilitating stiffness and pain. Tendonitis, especially in the elbow (commonly known as tennis elbow) or shoulder, is another frequent condition treated with cortisone infiltration. Bursitis, which occurs when fluid-filled sacs cushioning joints become inflamed, is also highly responsive to this therapy. Spinal conditions, including herniated discs or nerve root irritation, may benefit from epidural cortisone infiltrations, though these require even greater precision. Additionally, athletes often turn to cortisone infiltrations for acute injuries when inflammation prevents recovery, though careful monitoring is required to prevent long-term tendon damage. Physicians also use this treatment for plantar fasciitis, a painful foot condition affecting millions worldwide. Each condition responds differently to infiltration cortisone, making individualized medical assessment essential before proceeding.
The Procedure: Step-by-Step Insight
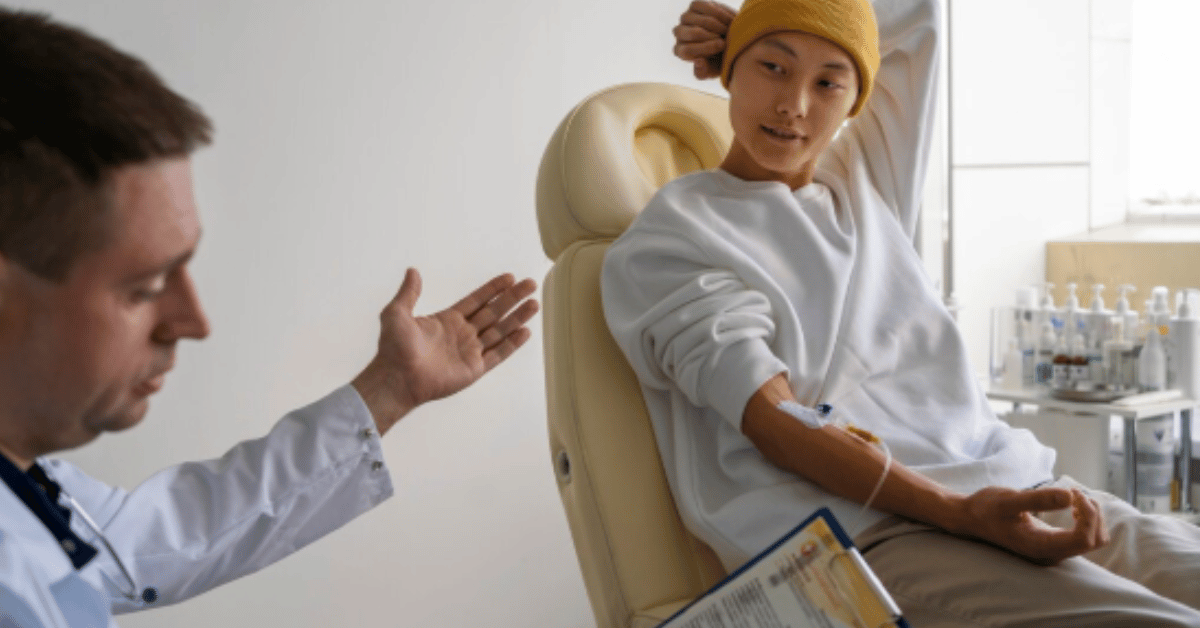
The process of receiving infiltration cortisone is relatively quick, often performed in a physician’s office or outpatient setting. First, the patient is positioned comfortably to expose the affected area. The physician cleans the skin with antiseptic to reduce infection risk, then may apply a local anesthetic to numb the site. Using either anatomical knowledge or imaging tools like ultrasound or fluoroscopy, the physician carefully guides the needle into the inflamed tissue or joint. Once placement is confirmed, the corticosteroid solution, sometimes mixed with a local anesthetic, is injected. The entire procedure typically takes less than 15 minutes, although patients are usually observed briefly afterward. Mild discomfort during the injection is common, but most report relief within days. For some, the effect is immediate due to the anesthetic, while for others, the steroid’s anti-inflammatory action builds gradually. Patients are often advised to avoid strenuous activity for at least 24 hours post-procedure, allowing the medication to settle into the targeted tissue.
Benefits of Infiltration Cortisone
The primary benefit of infiltration cortisone is rapid pain relief. Many patients experience a reduction in symptoms within days, allowing them to resume normal activities that had been limited by discomfort. This can be life-changing for individuals struggling with chronic joint pain, where every movement feels burdensome. Another benefit is improved mobility, as decreased inflammation translates into increased flexibility and range of motion. For those managing long-term conditions like arthritis, cortisone infiltration can delay the need for surgery, such as joint replacement. Furthermore, it reduces reliance on oral painkillers, particularly opioids, which carry a high risk of dependency and systemic side effects. Cortisone infiltration is also adaptable; it can be repeated when necessary, though with caution, to avoid potential tissue weakening. From an economic perspective, it is often more cost-effective than prolonged medication or surgical intervention. Ultimately, the ability to target inflammation precisely and provide sustained relief makes cortisone infiltration one of the most valuable tools in pain management today.
Risks and Side Effects of Infiltration Cortisone
Despite its benefits, infiltration cortisone carries certain risks that patients should carefully consider. Common side effects include temporary pain or swelling at the injection site, often referred to as a “cortisone flare,” which typically resolves within 48 hours. Skin thinning or changes in pigmentation near the injection site are possible with repeated treatments. More serious risks, though rare, include infection, tendon rupture, or damage to surrounding tissues. Long-term or excessive use of cortisone infiltrations can weaken ligaments and cartilage, potentially accelerating joint degeneration rather than preventing it. Diabetic patients may experience elevated blood sugar levels temporarily after injection, requiring careful monitoring. Systemic side effects are less likely compared to oral steroids, but still possible if high doses are used or injections are frequent. Physicians generally limit cortisone infiltrations to no more than three to four times a year in the same joint to minimize complications. As with any medical intervention, informed decision-making between doctor and patient is essential.
Comparing Cortisone Infiltration with Alternative Treatments
When evaluating cortisone infiltration, it is important to compare it with alternative approaches. Non-steroidal anti-inflammatory drugs (NSAIDs) are often the first line of defense, but they lack the localized precision of cortisone. Physical therapy offers long-term benefits by strengthening muscles and improving biomechanics, but progress is slower compared to the immediate relief from injections. Hyaluronic acid injections, another option for osteoarthritis, aim to lubricate the joint rather than reduce inflammation, making them more suitable for early-stage conditions. Platelet-rich plasma (PRP) injections, which use the patient’s own blood components to stimulate healing, have gained popularity as a regenerative option, though evidence is still developing. Surgical intervention remains the final step for severe cases when conservative measures fail. Each treatment has its strengths, and in many cases, physicians combine approaches for optimal results. Cortisone infiltration stands out for its speed and effectiveness, but it must be integrated thoughtfully into a holistic care plan.
Table 1: Key Conditions Treated with Infiltration Cortisone
| Condition | Common Target Areas | Expected Relief Duration | Notes on Effectiveness |
|---|---|---|---|
| Osteoarthritis | Knees, hips, shoulders | Weeks to months | Useful in moderate stages |
| Tendonitis | Elbows, shoulders, wrists | Weeks | Avoid excessive repeat use |
| Bursitis | Hips, knees, shoulders | Weeks to months | Effective in reducing swelling |
| Plantar Fasciitis | Heel and foot arch | Weeks | Requires supportive footwear |
| Spinal Disorders | Lumbar and cervical regions | Weeks to months | High precision required |
Recovery and Post-Treatment Care
Recovery after infiltration cortisone is relatively straightforward. Patients are typically advised to rest the treated area for 24 to 48 hours to avoid overexertion that could diminish the injection’s effect. Ice packs may be applied if discomfort or swelling occurs at the injection site. Most individuals can return to light activities the next day, though high-impact exercise should be delayed for several days. Long-term success often depends on complementary treatments such as physical therapy, weight management, or orthotic support. Physicians may recommend strengthening exercises once initial pain relief is achieved, helping to maintain joint stability and prevent recurrence of symptoms. Patients are also encouraged to track their pain relief duration, as this information guides future treatment planning. While cortisone infiltration can be repeated, careful monitoring ensures safety and effectiveness. Post-treatment care is not just about symptom management—it is also about making lifestyle changes that support joint and tendon health for the long term.
Table 2: Benefits vs. Risks of Infiltration Cortisone
| Aspect | Benefits | Risks/Limitations |
|---|---|---|
| Pain Relief | Rapid and targeted | Temporary flare possible |
| Mobility | Improved range of motion | Risk of tendon weakening |
| Frequency | Can be repeated if needed | Limited to a few times yearly |
| Cost | More affordable than surgery | Insurance coverage varies |
| Safety | Localized treatment, fewer systemic effects | Risk of infection, skin changes |
Patient Perspectives and Real-World Use
For many patients, infiltration cortisone represents a turning point in managing chronic pain. “I felt like I had my knee back after months of stiffness,” a patient once shared after a cortisone injection for arthritis. Such testimonials reflect the profound impact of targeted therapy on daily quality of life. Athletes recovering from tendonitis often describe cortisone infiltration as a tool that allowed them to continue training while addressing inflammation, though sports physicians emphasize the importance of cautious use. Patients with plantar fasciitis often recall being able to walk pain-free again after months of struggle. These narratives highlight that beyond medical terminology and technical details, infiltration cortisone restores something deeply human: the ability to move freely without constant pain. Yet, patients also recognize its limitations, acknowledging that injections are a bridge, not a final destination, in their broader journey of healing.
The Future of Infiltration Cortisone Therapy
The future of infiltration cortisone lies in balancing tradition with innovation. While cortisone remains a cornerstone of anti-inflammatory treatment, researchers are exploring how to minimize risks while maximizing benefits. Advances in biologics and regenerative medicine, such as stem cell therapy or enhanced PRP injections, may complement or gradually replace corticosteroids in certain contexts. Imaging technologies are also improving, making injections more precise and reducing complications. Moreover, new formulations of corticosteroids are being developed to extend the duration of relief while minimizing tissue damage. In clinical practice, the trend is shifting toward integrated care, where cortisone infiltrations are combined with rehabilitation, lifestyle coaching, and preventive medicine. “Medicine is moving from reactive relief to proactive restoration,” a rheumatologist recently remarked, capturing the evolving philosophy behind treatments like infiltration cortisone. While the therapy is here to stay, its role may transform into a stepping stone toward more regenerative and long-term solutions.
Conclusion
Infiltration cortisone continues to play a critical role in modern medicine by offering targeted, effective relief for inflammatory conditions that compromise mobility and quality of life. It is not a cure, but rather a therapeutic tool that provides valuable respite, often giving patients the strength to pursue longer-term strategies for recovery. Its benefits, including rapid pain relief and improved mobility, make it indispensable for many, though risks such as tendon weakening or infection underscore the importance of careful medical supervision. Patients considering cortisone infiltration should see it as part of a larger plan—one that includes lifestyle changes, physical therapy, and, when necessary, surgical options. As medicine evolves, infiltration cortisone remains a symbol of how targeted interventions can bridge the gap between discomfort and healing. Ultimately, the decision to use it should be guided by trust in medical expertise and an understanding of one’s personal health journey.
FAQs
Q1: How long does pain relief from infiltration cortisone last?
Relief can last from several weeks to a few months, depending on the condition and patient response.
Q2: Can infiltration cortisone cure arthritis?
No, it cannot cure arthritis. It helps manage inflammation and pain, but the underlying joint damage remains.
Q3: How many cortisone infiltrations can I receive in a year?
Most physicians recommend no more than three to four injections per year in the same joint.
Q4: Is infiltration cortisone safe for diabetic patients?
Yes, but it may temporarily raise blood sugar levels. Close monitoring is necessary after the injection.
Q5: What should I avoid after receiving cortisone infiltration?
Strenuous activities should be avoided for 24–48 hours to allow the medication to take full effect.